Breast pain, or mastalgia, is discomfort, tenderness, tightness or pain in the breast or underarm region. Mastalgia is a common condition among women and usually is NOT a common symptom of breast cancer. Breast pain is more common in younger women who have not completed menopause, but postmenopausal women sometimes experience breast pain. Some common sources of breast pain include:
- Benign cysts. These fluid-filled sacs can be soft or hard and commonly enlarge during the menstrual cycle and go away after menopause
- Menopause
- Menstruation and premenstrual syndrome (PMS)
- Pregnancy – more common in the first trimester
- A breast abscess, or small infection inside of the breast
- Medications that affect reproductive hormones, some cardiovascular treatments, and some mental health treatments. Known triggers include: oral contraceptives, antidepressants, certain diuretics, anadrol, digitalis preparations, methyldopa (Aldomet), spironolactone (Aldactone), and chlorpromazine
- Improperly fitted bras can compress or improperly support breasts, leading to discomfort
- Costochondritis: inflammation of the cartilage that connects the ribs and breastbone. Often affects individuals over the age of 40 and can occur with arthritis, injury, or physical strain
- Fibrocystic breast changes can cause swelling and lumpiness in the breasts, due to buildup of fluid-filled cysts and fibrous tissue. This is not linked to breast cancer and is common among women 20-50 years old. Following low-salt diets and using mild pain-relief medication may reduce discomfort
- Mastitis is an infection of the breast, commonly due to a clogged milk duct from breastfeeding but may have other sources. Symptoms often include fever, aches, and fatigue
- Breast cancer is often not associated with breast pain, however, inflammatory breast cancer and some tumors can lead to breast discomfort
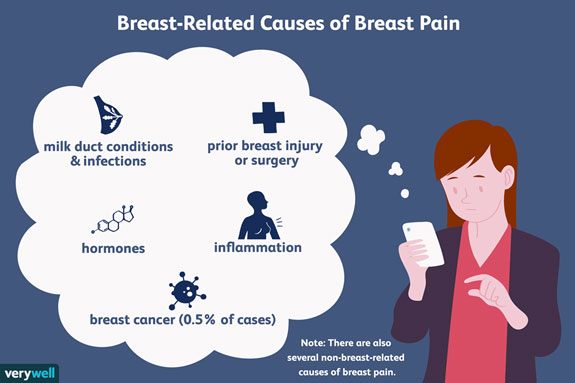
Illustration by Emily Roberts, Verywell
Cyclic pain, which accounts for 75 percent of breast pain, is linked to menstruation and results from monthly fluctuations of estrogen and progesterone. Hormone levels can increase the size and number of ducts and milk glands, causing the breast to retain water. Leading up to menstruation, it is common for the breasts to swell and become swollen, heavy, or tender. Symptoms typically resolve at the end of menstruation. Hormonal changes during pregnancy and breastfeeding may also induce breast changes and pain. During perimenopause, cyclic pain may worsen, due to dramatic surges and drops of hormone levels.
Noncyclic pain is unrelated to the menstrual cycle or hormonal changes. Noncyclic pain may be intermittent or constant, affect one or both breasts, and involve the entire breast or just a portion. It can feel like a tightening, soreness, or burning and is often a symptom of a specific problem, including trauma, benign tumor, cyst, former biopsy, or conditions in underlying structures (neck, upper back, chest wall, esophagus, or heart).
Treatment for breast pain will vary on whether your pain is cyclical or noncyclical. If your pain persists and keeps you from daily activities, consider speaking to physician about treatment options, including:
- Reducing sodium intake
- Calcium supplements
- Wearing a supportive bra
- Oral contraceptives to regulate hormone levels
- Fish oil supplements
- Estrogen blockers, such as tamoxifen
- Pain relievers (NSAIDs), such as ibuprofen or acetaminophen
Breast pain is not usually related to breast cancer, however, you should contact your healthcare provider if you experience pain along with any of the following symptoms:
- Bloody or clear discharge from the nipple
- A new lump that does not go away after your menstrual cycle
- Persistent breast pain with no known cause
- Local redness, pus, or fever – indicating breast infection
- Redness of the skin of the breast. May appear as a rash, dilated pores, and possible skin thickening. These may be signs of inflammatory breast cancer
Resources
“10 Common Causes of Breast Pain.” Medical News Today. MediLexicon International, November 21, 2018. https://www.medicalnewstoday.com/articles/311833.
“Breast Pain.” Mayo Clinic. Mayo Foundation for Medical Education and Research, January 31, 2019. https://www.mayoclinic.org/diseases-conditions/breast-pain/symptoms-causes/syc-20350423.
“Breast Pain.” National Breast Cancer Foundation, September 28, 2020. https://www.nationalbreastcancer.org/breast-pain/.
Herndon, Jaime. “Breast Pain: Types, Causes, and Treatments.” Healthline. Healthline Media, May 13, 2019. https://www.healthline.com/symptom/breast-pain.
Publishing, Harvard Health. “Breast Pain: Not Just a Premenopausal Complaint.” Harvard Health, July 7, 2020. https://www.health.harvard.edu/pain/breast-pain-not-just-a-premenopausal-complaint.
Stephan, Pam. “Possible Reasons Behind Your Breast Pain,” November 7, 2019. https://www.verywellhealth.com/causes-for-sharp-breast-pain-429843.
———. “Is It Normal to Have Breast Pain During Your Period?” Verywell Health, December 2, 2019. https://www.verywellhealth.com/breast-pain-and-your-menstrual-period-429841.